When I found out I was pregnant again, so much had changed since the last time that I felt a little unsure of what to do next. We had moved, I was now also living with another autoimmune disease which had triggered a physical change in me including a massive increase in my weight. I felt out of my comfort zone and whilst excited and fortunate beyond words to be adding another tiny human to the clan, I was anxious in a way I’d never felt before.

Where we live now there’s an online self referral form when you find out you’re expecting. This seems to go to a central team who then allocate you to a community midwife and who should refer you to appropriate consultant led care if the information is there to begin with, which of course mine was. I should have received an appointment from the Diabetes team (who were not MY usual diabetes team) at the local hospital much sooner than the 8 weeks it took. (I found out I was pregnant really early, like just over a week after conception early). The only indication I’d had from the central team that I’d need consultant led care was a letter stating that because my BMI was high, I was considered high risk and would need to be under consultant led care at the complex pregnancy clinic (I really don’t like that name btw)! By this point, I’d already had a telephone booking in appointment and had asked for the appropriate referrals to be made as my husband and I had decided to give the new area a go, rather than travel the almost 2 hours back and forth to Oxford for appointments. That feels like such a huge mistake now with the power of hindsight.
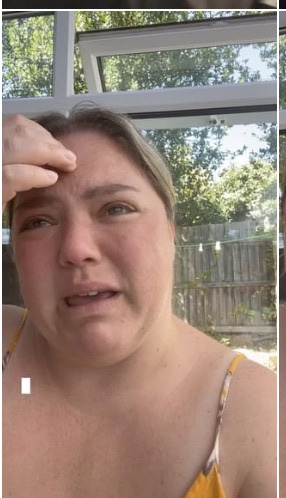
After what seemed like a labyrinth of admin teams, I eventually had an appointment through, a telephone appointment! For someone they’d never met and who was new to their service, and had already had her anxiety increased by their lacklustre performance, a telephone appointment! OK, I thought, we’ll roll with it and hopefully it’ll be fine, if all else fails I’ll ask if Oxford will have me back. The day of the appointment came around and having felt so empowered by both of the community midwives I’d encountered so far, I actually felt excited to virtually meet the new team. I would have 2 calls, one with an obstetrician and one with a diabetes specialist nurse and consultant. For those who follow me on instagram, you may recall the tearful and distressed insta stories back in the summer, the tale of the horrific experience; well that was this day!
In a phone call lasting 12 minutes, the obstetrician unnecessarily mentioned my BMI over 8 times that I counted, there was no clinical reason for it AT ALL to be mentioned so frequently. She was not receptive to my desire to talk about the possibility of a VBAC and to not make any firm decisions so early in the pregnancy about mode of birth, or the reasons why that was important to me, in fact she told me all of the worse case scenarios in horrifically, and unrequested graphic detail, without acknowledging that these are risks, not givens. This obstetrician, looked at a series of numbers on a page and made a judgement about me which was unwarranted and downright dangerous. As a healthcare professional, I was shocked that amongst her thought processes she had not considered the facts that A) I was diagnosed with Hashimoto’s Thyroiditis around 6 months previously, a symptom of which is weight gain! B) She had not accounted for the fact that the majority of people living with Type 1 Diabetes also live with many mental and emotional burdens, one of which is a difficult relationship with food, which can trigger eating disorders or periods of disordered eating. I was certainly triggered after the phonecall and found myself feeling judged, it felt like she was telling me I shouldn’t be having a baby because I wasn’t a decent enough human being, but a broken one who would inflict danger upon my unborn child and would likely never meet it because I would probably die in childbirth if I didn’t agree to another c-section just because she said so. I have been very open about my mental health and body image struggles both publicly and with my HCPs, it is clearly on the records from my booking in appointment and would have been available for the obstetrician to see. Her behaviour towards me devastated me, but this was just the beginning, the diabetes call was yet to come….
Just over an hour later, my phone rang again. I wiped away my tears, took a deep breath and naively thought this will be different. I thought that most diabetes teams now know about the importance of Language Matters and the principles behind it, use it in their everyday practice and understand the benefits of a person first consultation…. Oh my goodness how wrong I was!! Again, with hindsight I ask myself if I was a fool to expect more given the experience I’d had within the last 90 minutes? The eternally hopeful optimist in me says no, because if I’d answered the phone believing that then the conversation which followed would have been worse….and my fault. I don’t know where to begin with this one. I’ll start by acknowledging my privilege that Oxford are, in my honest opinion an incredible team. They know me, they know my diabetes and they have already supported me through 2 very wonderful pregnancies and into parenthood. They are patient led in my experience and have genuine care for the impact they can make and the part they play in “The Team”. My diabetes consultant during pregnancy also happens to be one of the co-authors on the NHS Language Matters document and has given me opportunities to speak about my experiences with SpRs and beyond. I wish everyone could have the experiences I have with Oxford because it’s honestly so empowering, and on those rare occasions when it’s not been as I’d hoped, they’ve been open to the feedback and what would work better for me. I know how absolutely privileged I am, I really do.
So, to begin my very first encounter with the Diabetes Specialist Team with questions along the lines of, “You’re a type 1 diabetic, what’s your control like?”. “Do you take insulin for your diabetes?”, “Do you know the sick day rules?”, “Have you been checking for ketones when you’re over 10mmol?” and “Why haven’t your sugars been within 3.8 to 5mmol consistently in the last 2 weeks?”. For a start, don’t call me a diabetic because that’s a sure fire way to get me on the back foot, especially when phrased like that!! You’re unlikely to ever hear me refer to “my sugars”, I find it’s misleading especially in a world where PLWD are still trying to explain we can eat sugar and it is infact carbs we need to monitor. The word “control” implies that Diabetes is something that can be controlled, tamed, not a burden if you put the effort in. Theres an implication with the world control that just doesn’t apply to life with T1D, which is why I talk about management. Do I know the sick day rules…by this point I felt like I was teaching a language matters seminar! Do I know the sick day rules, I’ve already told you I’ve lived with T1D for almost 22 years and you can see I’m over 40 with 2 autoimmune conditions, if I didn’t know the sick day rules would I be talking to you on the phone about my 3rd pregnancy?????? It was just disastrous, and on top of that came the realisation that I’d probably spend more time during this pregnancy introducing my diabetes to people than I would actually getting the support I needed. I also didn’t want to feel like a broken record, my usual tactic when it comes to introducing my language preferences around my diabetes is to repeat what they’ve said using my preferred terms, so “You’re diabetic” gets “Yes, I live with Type 1 Diabetes” and so on and so forth. I feel it’s a less confrontational way of doing things but also gives examples of how to employ Language Matters within conversations. I could of course, and I have, signpost to the Language Matters document, but you also can’t beat real life experience, although this was not how I wanted to spend my pregnancy. The consultant then insisted he wanted me to attend weekly face to face clinics, which wouldn’t work for me given the childcare needs and my husbands working pattern, especially when you can’t take your children into clinic with you. Weekly also felt really excessive to me, not to be boastful, but this wasn’t my first rodeo and I’d picked up a few things on the previous rides, including how to ask for help if I needed it between appointments. I tried to explain my thoughts on this to the consultant, but he was having none of it, then it was like speaking to the obstetrician again; “because you’re a geriatric mother with a high BMI and you’re diabetic we need to see you or at least speak to you weekly and we need to see your cgm traces so we can call you if you go high”. I could feel a rage about to erupt in me and I’ve no idea how I managed this, through gritted teeth I simply repeated that I would not be able to attend face to face appointments weekly, the reason why and also explaining that I have lived with T1D for 22 years, have had 2 healthy and successful pregnancies and at this point in my 3rd pregnancy, I did not feel out of my comfort zone, but if they could ensure I have contact details then I would be in touch the minute I needed their help. I also promised (with fingers crossed behind my back) to accept their invitation to share my CGM with them. It worked this time, we made an appointment for the future and I thought to myself “just need to say bye and hang up and then I can let this rage out”. Nope, the DSN wanted to repeat some of the questions the consultant had asked! I don’t think I’ve ever been aware of my blood pressure rising before, but thank god for Felix waking up from his nap at this point because I simply said “Sorry, my son needs me. Bye” and honestly I don’t think I’ve ever appreciated the connection with another human being as much I did the one I have with my little dude in that moment. I had never felt so judged or disconnected with HCPS, well not since my late teens/early 20’s, I felt unequal and that’s not the way a team works, it’s certainly not the way the team I have at Oxford work and it sat so uncomfortably with me that I spent the remainder of the day in a really unpleasant state of distress.
The impact of this didn’t just mean I sent an email to my community midwife and Oxford stating I wished to transfer my consultant led care back there, but it has left me with a lingering anxiety that has grown throughout my pregnancy. I’ve always known that pregnancy and Type 1 Diabetes carry higher risk factors, and I’ve spent a lot of time reassuring myself through research and peer conversations that those risk factors were not forgone conclusions. In my early years living with T1D the thought of not being able to become a mother was pretty much the first thing I questioned, I didn’t get reassurance from the retirement age male consultants I saw, no information about the connection between female hormones and cycles on my BGs; in fact one man told me not to even think about getting pregnant with an HBA1C like mine – I don’t think I was even a year into my diagnosis at that point, I certainly hadn’t had any education. I’ve spent time advocating for better conversations around pregnancy and diabetes, and I feel I’ve spent even more time trying to dispel the stereotypes; the giant baby, the highly medicalised labour and birth as the only option, a pregnancy devoid of “normality” and the joy every expectant parent deserves to feel… and here I am, fearing worst case scenarios because of the carelessness of language used by HCPs who didn’t take the time to get to know me and put my experience at the forefront of their assessments and the support they offer. I maintain throughout any peer support I give, that building the right team of HCPs around you when you’re living with Diabetes, and even more so when experiencing pregnancy and then parenthood is as important as the right tools for managing your BGs. I respect the decision my HCPs have made to specialise and study Diabetes, the time they spend keeping abreast of latest research, various technologies and how they acknowledge the impact living day to day with Diabetes has. They in turn respect the hard work I put in and the experience I have within MY diabetes, it is an opportunity to learn from each other and find ways to work together towards the same outcome; me living well emotionally and physically, with T1D.
So where am I now? I’m almost at the end of my pregnancy, I have had the conversations about why I came into this pregnancy wanting a VBAC and during those had the opportunity to explain that in fact, the mode of birth wasn’t the concern for me. I had no aspirations of birthing in a lilly pond with floating candles with a view of a desert sunset mural and a carefully curated soundtrack playing in the background. I began with my recovery (if you can call them that) from my previous 2 c-sections and made it clear that I cannot repeat those experiences for the sake of Tabitha, Felix and Matt. Bingo! That was the issue. This enabled me to lead conversations about a better recovery plan and fortunately, the team at Oxford have been supportive and understanding. They’re monitoring my anxieties and doing their utmost to reassure and collaborate on a recovery plan whilst I’m in hospital alongside working out the support I might need when I get home as well as in the run up to the birth of Flump. We have agreed a c-section is the safest option given my history (failed induction became an emergency c-section, then a planned c-section during a pandemic..) but also for us it means we can be practical about things and make arrangements for the Best Big Sister in the world and the Little Big Brother to be, who has obviously learned from the best. I won’t lie, knowing the date (no, I’m not sharing it far and wide, I like to maintain some mystery) does put a bit of pressure on the To Do list, and both Matt and I feel unprepared in ways but the practicality of it is a bit of a perk.
The pregnancy itself has felt harder at points, we moved home in spring last year and there has been lots of stress in trying to get things done in the house. I won’t bore you with the details, but although we’re very settled here we’ve not really finished unpacking and there is an ongoing legal situation with a contractor. Our daughter started school and then we hit Xmas – no one tells you how many social events there are at school in the run up to Christmas, it should definitely be in the prospectus! Our son started nursery and has overcome much of his separation anxiety, but I’ve missed him. All this has meant that my BGs have had cortisol to contend with on top of the multitude of other challenges faced when managing BGL’s whilst pregnant. I’ve always been reactive and worked hard to maintain my Time in Range, but I have to admit to not having as much time or mental space at points to give it the focus I could in my first pregnancy. But, Flump is incredibly active and so far seems to be following the same growth trajectory as their brother and sister and I guess now it’s just a matter of time before I find out if I’ve done enough to minimise or even negate all those risks the team I’m no longer with, made so prominent in their consultations. I know I’ve put the effort in, I’ve been on the same page as my team with things that need tweaking at pretty much every appointment and perhaps it’s not that I’ve lacked time or mental space, but that maybe, after 2 pregnancies I know more about my body, my diabetes and my baby’s needs than I give myself credit for….
In short, so far the third time hasn’t felt very charming at points, but I do feel a great deal of privilege to be doing this again, to feel empowered by knowledge and experience and to have built a great support team from antenatal to postpartum, including physio and infant feeding, and maybe that’s the charm of it…
See you all on the other side…..we may even have a name for this baby by then!
Nxx
